Pain is a complex and multifaceted sensory and emotional experience that serves as a crucial protective mechanism for organisms. It is defined by the International Association for the Study of Pain as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”[1].
The primary functions of pain include:
- Motivating organisms to withdraw from harmful situations
- Protecting damaged body parts during healing
- Encouraging avoidance of similar experiences in the future
Pain can be classified in several ways:
- By duration:
- Acute pain: Short-term pain that typically resolves once the underlying cause is addressed
- Chronic pain: Persistent pain lasting for extended periods, often beyond the expected healing time
- By type:
- Nociceptive pain: Caused by tissue damage or potential tissue damage
- Neuropathic pain: Resulting from damage or dysfunction in the nervous system
- Psychogenic pain: Pain influenced by psychological factors
- By location:
- Localized pain: Confined to a specific area of the body
- Referred pain: Felt in a location different from its origin
Pain can manifest in various forms, including:
- Allodynia: Pain experienced in response to normally non-painful stimuli
- Phantom pain: Pain felt in a part of the body that has been amputated
- Breakthrough pain: Sudden, intense pain that “breaks through” regular pain management
The experience of pain involves complex neurological processes:
- Nociceptors in the periphery detect noxious stimuli
- Pain signals travel along A-delta (fast, sharp pain) and C fibers (slow, dull pain)
- Signals reach the spinal cord and ascend to the brain via the spinothalamic tract
- The brain processes pain information in multiple areas, including the thalamus, insular cortex, and anterior cingulate cortex
Pain assessment and management are crucial aspects of healthcare. Assessment tools include:
- Numerical rating scales (e.g., 0-10 pain scale)
- Visual analog scales
- Verbal rating scales
- McGill Pain Questionnaire
Pain management strategies can be broadly categorized into:
- Pharmacological interventions:
- Analgesics (e.g., NSAIDs, opioids)
- Adjuvant medications (e.g., antidepressants, anticonvulsants)
- Non-pharmacological interventions:
- Physical therapy
- Cognitive-behavioral therapy
- Mindfulness and relaxation techniques
- Acupuncture
- Interventional procedures:
- Nerve blocks
- Spinal cord stimulation
- Radiofrequency ablation
The impact of pain extends beyond physical discomfort, affecting various aspects of an individual’s life:
- Cognitive function: Impaired concentration, working memory, and problem-solving abilities
- Emotional well-being: Increased risk of depression, anxiety, and irritability
- Quality of life: Interference with daily activities, work, and social relationships
Pain has been a subject of scientific inquiry and philosophical debate throughout history. Ancient theories attributed pain to imbalances in bodily fluids, while modern understanding is based on neurobiological mechanisms[1].
The evolutionary perspective on pain suggests that it serves as a vital survival mechanism, protecting organisms from harm and promoting healing. However, chronic pain conditions that persist beyond their protective function pose significant challenges to this evolutionary model[1].
In conclusion, pain is a complex phenomenon that involves sensory, emotional, and cognitive components. Its understanding and management require a multidisciplinary approach, considering both biological and psychosocial factors. Ongoing research continues to unravel the intricacies of pain mechanisms, paving the way for more effective treatments and improved quality of life for those experiencing pain[1].
[glossary_wikipedia]
Pain is a distressing feeling often caused by intense or damaging stimuli. The International Association for the Study of Pain defines pain as "an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage."
| Pain | |
|---|---|
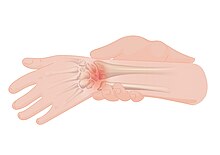 | |
| An illustration of wrist pain | |
| Specialty | Neurology Pain medicine |
| Symptoms | Unpleasant sensory and emotional sensations |
| Duration | Typically depends on the cause |
| Types | Physical, psychological, psychogenic |
| Medication | Analgesic |
Pain motivates organisms to withdraw from damaging situations, to protect a damaged body part while it heals, and to avoid similar experiences in the future. Most pain resolves once the noxious stimulus is removed and the body has healed, but it may persist despite removal of the stimulus and apparent healing of the body. Sometimes pain arises in the absence of any detectable stimulus, damage or disease.
Pain is the most common reason for physician consultation in most developed countries. It is a major symptom in many medical conditions, and can interfere with a person's quality of life and general functioning. People in pain experience impaired concentration, working memory, mental flexibility, problem solving and information processing speed, and are more likely to experience irritability, depression, and anxiety.
Simple pain medications are useful in 20% to 70% of cases. Psychological factors such as social support, cognitive behavioral therapy, excitement, or distraction can affect pain's intensity or unpleasantness.
English
Etymology 1
From Middle English peyne, payne, from Old French and Anglo-Norman peine, paine, from Latin poena (“punishment, pain”), from Ancient Greek ποινή (poinḗ, “bloodmoney, weregild, fine, price paid, penalty”).